Microflap surgery is a delicate procedure to remove benign growths on the vocal cords, such as cysts, polyps, or other cysts, while preserving the surrounding vocal tissue. During this surgery, the doctor creates a tiny flap in the surface of the vocal fold, gently lifts it, and removes the lesion beneath. This method minimizes scarring and preserves the patient's voice quality.
The procedure is performed under general anesthesia using a microscope and microsurgical tools. After surgery, patients are usually placed on strict voice rest for a few days, followed by a gradual return to speaking. Voice therapy is often recommended to optimize healing and prevent recurrence. Risks include scarring, temporary hoarseness, or, less commonly, changes to voice quality. Recovery is usually smooth, and the surgery often significantly improves vocal function.
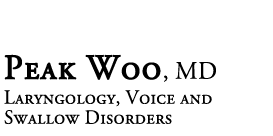
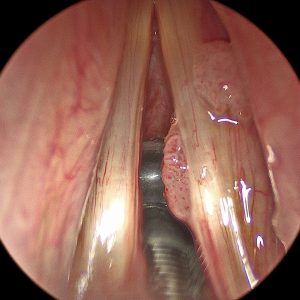
Before: Microflap Surgery for a Vocal Fold Cyst

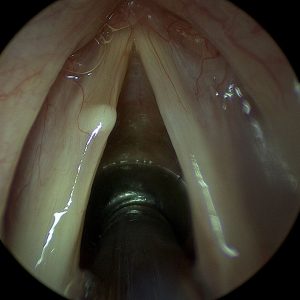
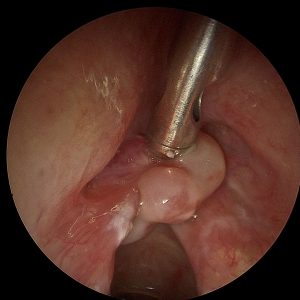
After: Microflap Surgery for a Vocal Fold Cyst
Microlaryngoscopy with excisional biopsy involves surgically removing a small piece of tissue from the vocal cords or larynx to be examined under a microscope. It is used when an unknown lesion or abnormality, such as a nodule, mass, or ulcer, is present and a precise diagnosis is needed.
This procedure is done under general anesthesia using specialized tools through the mouth. Through a microscope, the surgeon views the vocal cords and carefully removes the target tissue. Afterward, patients are typically advised to rest their voice and may feel mild throat discomfort. Results from the biopsy usually guide further treatment. The risk of complications is low, and speech is usually unaffected once healing is complete, though some patients may need follow-up procedures or therapy based on the biopsy results.
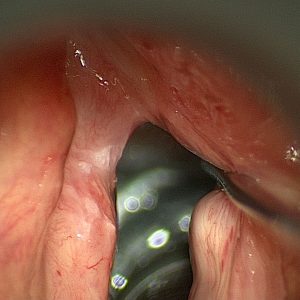
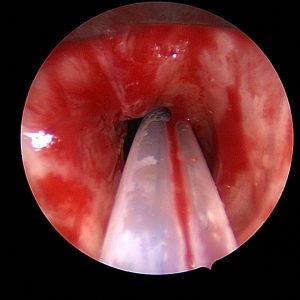
Before: Microlaryngoscopy removal of Leukoplakia
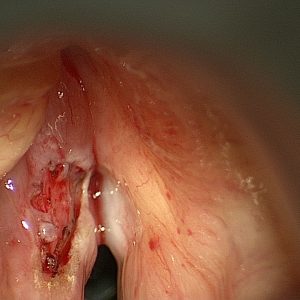
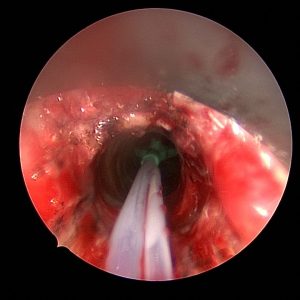
After: Microlaryngoscopy removal of Leukoplakia
This procedure involves using a CO2 laser to remove papillomas—wart-like growths caused by the human papillomavirus (HPV)—from the vocal folds. If they grow large or recur, papillomas can cause hoarseness, voice changes, and breathing issues. Laser excision allows for precise removal of these lesions while preserving surrounding healthy tissue.
Under general anesthesia, the surgeon uses a micro laryngoscope to access the vocal folds and a CO2 laser to vaporize or cut away the papillomas. This technique is less invasive and allows for quicker recovery with minimal bleeding. Patients are advised to rest their voice following surgery and may need repeated procedures if the papillomas return. Risks include temporary hoarseness, vocal cord scarring, or recurrence of the papillomas, which is common in some cases due to the viral nature of the disease.
Before: CO2 Laser Excision of Papilloma

After: CO2 Laser Excision of Papilloma
Laser cordectomy is a surgical procedure that uses a precise laser beam to remove cancerous tissue from the vocal cords. It is often performed in early-stage laryngeal cancer, where preserving voice and airway function is important. Depending on the amount of tissue that needs to be removed, the procedure is categorized into types I through VI.
Performed under general anesthesia, the surgeon uses a laser to excise the cancerous areas while minimizing damage to surrounding structures. The more extensive the resection (higher type number), the greater the impact on voice. Recovery includes a period of voice rest and follow-up visits to monitor healing. Some patients may notice a permanent change in voice quality, and voice therapy may be recommended. The procedure avoids more invasive surgery or radiation in many cases, making it a preferred option for early laryngeal cancer.
Before: Trans Oral Laser Cordectomy for Cancer

After: Trans Oral Laser Cordectomy for Cancer
This combined procedure treats laryngeal stenosis, a narrowing of the airway that can cause breathing and voice problems. The CO2 laser is used to carefully remove scar tissue or abnormal growths, and dilation stretches the airway open to restore normal airflow.
Surgery is done under general anesthesia using a microscope and laser equipment. Balloon or rigid dilators may be used to expand the narrowed area. Postoperative care often includes voice rest, steroid or anti-inflammatory medications, and sometimes repeat procedures. Risks include recurrence of the stenosis, temporary voice changes, and airway irritation. This approach helps improve breathing while preserving voice as much as possible.
Before: CO2 Laser Excision for Stenosis
After: CO2 Laser Excision for Stenosis
This procedure improves vocal cord function in patients with vocal cord atrophy, scarring, or paralysis. Fat is harvested from another part of the patient's body—often the abdomen or thigh—and carefully injected into the vocal cord to restore bulk and improve closure during speech. This fat injection helps improve voice strength and reduce breathiness.
The procedure is done under general anesthesia using an operating microscope. A small incision is made to harvest fat, which is then purified and injected precisely into the vocal fold. Recovery typically includes voice rest for several days, and voice therapy is often recommended afterward to help optimize vocal performance. Some of the injected fat may be absorbed over time, so occasional touch-up procedures may be needed. Most patients experience a noticeable improvement in vocal strength and endurance.
VoiceGel is a biocompatible, temporary filler injected into the vocal fold to improve vocal cord closure. It's commonly used for temporary vocal fold paralysis, vocal cord weakness, or diagnostic purposes to assess if a more permanent injection will benefit. The gel provides immediate voice improvement and naturally resorbs over a few months.
During this procedure, which is performed under general anesthesia, the surgeon uses a micro laryngoscope to view the vocal folds and inject the material with precision. Patients typically notice an improvement in voice quality soon after the procedure. Since it is temporary, the effects wear off over time, making this a good option for short-term correction or trial before a permanent solution. Recovery involves limited voice use and close follow-up to assess results.
Cidofovir is an antiviral medication used to treat recurrent respiratory papillomatosis (RRP), a condition in which benign HPV-related growths develop in the airway. During this procedure, after removing the papillomas (often with a laser), the surgeon injects Cidofovir directly into the affected area to help reduce the recurrence of the disease.
The injection is done during microlaryngoscopy under general anesthesia. It is often part of a long-term management plan for patients who experience frequent recurrences of papillomas. Recovery is similar to other microlaryngoscopy procedures involving voice rest and follow-up endoscopic evaluations. While Cidofovir is not a cure, it can decrease many patients' severity and frequency of outbreaks.
Steroid injections are used to reduce inflammation, scarring, or swelling in the vocal folds. They are commonly given to patients with chronic laryngitis, vocal fold nodules, granulomas, or after vocal fold surgery to help promote healing and reduce scar tissue formation.
The steroid is injected directly into the vocal fold tissue. The medication helps calm inflammation and support smoother, more flexible vocal cord movement. Patients typically follow up with voice rest and therapy. This low-risk approach is often used to enhance recovery from other vocal cord surgeries or treat specific voice-related inflammatory conditions.
This procedure treats vocal cord scarring, thinning, or atrophy that affects voice quality. PRP (Platelet-Rich Plasma) and fat are both natural substances derived from the patient's own body. Fat can help restore lost volume and cushion the vocal folds, while PRP, which is rich in growth factors, supports tissue healing and regeneration. When used together, they can improve vocal fold pliability and vibratory function, leading to a stronger, clearer voice.
The procedure is done under general anesthesia using a surgical microscope. A small incision is made in the vocal fold surface, and fat (usually harvested from the abdomen or thigh) and/or PRP are injected into the vocal fold muscle. Recovery typically involves voice rest for several days to allow the tissues to settle and heal. Most patients gradually resume speaking, and the voice often improves over several weeks. Follow-up may include voice therapy to optimize the results. Because fat may be reabsorbed over time, some patients may need a second procedure later.
This procedure is most commonly used to treat spasmodic dysphonia, a voice disorder in which the vocal cords involuntarily spasm during speech. Botox (botulinum toxin) is a well-established treatment that temporarily weakens the overactive muscles, allowing for smoother, more controlled speech. Botox may also be used in select cases of vocal tremor or other laryngeal dystonias.
When performed under general anesthesia with a laryngoscope and surgical microscope, this procedure allows for precise placement of Botox into the vocal muscles. It is generally very safe and takes only a few minutes. Afterward, patients may experience temporary breathiness, reduced vocal strength, or mild swallowing difficulty, which usually resolves within a few days to weeks as the muscles adjust. The full benefit typically appears within a week and lasts around 3–6 months. Repeat injections are often needed to maintain voice improvement.
Microlaryngoscopy with Botox injection for Abelchia (inability to burp) is a specialized surgical procedure to help patients who are unable to belch due to tightness or dysfunction of the cricopharyngeus muscle,a component of the upper esophageal sphincter. Under general anesthesia, a rigid laryngoscope is used to access the upper airway, and a small amount of botulinum toxin is precisely injected into the cricopharyngeus muscle. This weakens the muscle just enough to allow trapped air to be released, relieving symptoms such as bloating, gurgling, chest pressure, and abdominal discomfort. The procedure is performed on an outpatient basis, and most patients go home the same day. Recovery is generally quick, and patients can return to a normal diet as tolerated. Many people begin to burp within a few days to a week, with symptom relief often continuing for several months or longer.
The following video is a patient one week after Botox injection. She complains of some swallow dysfunction but is happy she can belch again.
KTP (potassium titanyl phosphate) laser ablation treats vascular lesions, papillomas (caused by HPV), or certain benign and malignant vocal fold growths. The KTP laser is unique because it targets blood vessels, allowing for precise treatment of lesions with minimal damage to the surrounding tissue — making it an excellent tool for preserving vocal quality.
During the procedure, the patient is placed under general anesthesia, and a laryngoscope is used to expose the vocal folds. The surgeon then uses the KTP laser, delivered through a thin fiber, to gently shrink or remove the lesion. Because it causes less thermal damage than other lasers, healing is typically quicker, and voice outcomes are often excellent. Patients usually need voice rest for a few days afterward, followed by a gradual return to speaking. In some cases, especially with papillomas, multiple treatments may be necessary. Follow-up may include repeat scopes and voice therapy.
This advanced procedure repairs areas of damaged or missing vocal fold tissue. It is often performed in cases where previous surgery, trauma, or disease has caused scarring or tissue loss, leading to a stiff, breathy, or hoarse voice. The goal is to restore the smooth mucosal surface of the vocal fold to vibrate properly for sound production.
Under general anesthesia, the surgeon uses a microscope and delicate instruments to remove scarred or damaged areas. A small graft — often taken from the patient’s own mouth lining (buccal mucosa) — is then precisely placed over the area to replace the lost tissue. After surgery, patients are usually asked to rest their voice for at least a week. Recovery also involves follow-up with laryngoscopy to check healing, and often voice therapy to retrain the voice. Results can be excellent but may take time to fully develop.
This procedure improves vocal quality by adjusting the position or tension of the vocal folds. It is typically used to treat vocal fold paralysis, weakness, or asymmetry that causes a breathy or weak voice. During microlaryngoscopy, laryngoplasty techniques are performed internally — often by injecting material or reshaping vocal structures to improve closure and voice production.
Performed under general anesthesia, the vocal folds are accessed through the mouth using a surgical microscope. The surgeon may inject fat, filler or use sutures or implants to reposition the folds. The results can lead to better vocal strength, clarity, and endurance. Most patients recover quickly, with some voice rest required. The voice often improves within days, but optimal results are usually seen over several weeks. Risks are minimal, and follow-up includes voice therapy to help the patient adapt to the new vocal mechanics.
This combined procedure treats Zenker’s diverticulum, a pouch that forms in the upper esophagus and traps food. This can lead to difficulty swallowing, coughing, and even aspiration (food entering the airway). The surgery also involves cutting the cricopharyngeal muscle, which can become overly tight and contribute to the problem.
Performed under general anesthesia, the surgeon accesses the pouch through the mouth or neck and divides the wall between the esophagus and the pouch (diverticulotomy), allowing food to flow normally. At the same time, the tight muscle at the upper esophagus is cut (myotomy) to reduce pressure and prevent recurrence. Most patients notice improvement in swallowing. Recovery involves a short hospital stay, starting with a liquid diet that gradually advances. Risks include bleeding, infection, or temporary hoarseness, but complications are uncommon in experienced hands.
Tubed supraglottoplasty is a procedure to treat laryngomalacia and aspiration, a condition where soft tissues above the vocal cords collapse inward during breathing, causing noisy breathing or airway obstruction — most common in infants and young children. This surgery reshapes or stiffens those tissues to improve airflow. When done for aspiration, the height of the larynx is changed to prevent spillover of food and liquids into the larynx.
During the procedure, which is done under general anesthesia, a laryngoscope is used to access the upper larynx. The surgeon carefully trims or repositions floppy tissue, often creating a differently shaped airway. Sometimes, tiny tubes (stents) are temporarily placed to hold the tissues in their new position as they heal. Recovery depends on the age and condition of the patient, but many experience immediate improvement in breathing and feeding. Postoperative care includes close monitoring for airway swelling and follow-up laryngoscopy. In most cases, voice and swallowing are unaffected or improve as breathing normalizes.
This procedure involves harvesting a small section of the inner cheek lining (buccal mucosa) as a graft to repair or reconstruct parts of the airway or vocal cords. It's often used when significant tissue loss, scarring, or stenosis (narrowing) in the throat or larynx cannot be repaired with local tissue alone.
Under general anesthesia, a graft is removed from the inside of the cheek — an area that heals quickly — and is then shaped and sutured into the affected area. The goal is to restore normal structure and function while minimizing voice or airway compromise. Recovery involves voice rest, wound care, and sometimes temporary stents or breathing support, depending on the location of the graft. Voice therapy and follow-up scopes are essential to guide healing. The donor site in the mouth may feel sore for a few days but generally heals without long-term issues.
A split-thickness skin graft involves taking a thin layer of skin from one part of the body (usually the thigh) and using it to reconstruct another area that has lost skin or tissue. In laryngology, it may be used to cover large mucosal defects in the throat, trachea, or neck following tumor removal or trauma.
The surgery is performed under general anesthesia. The graft is harvested, placed over the defect, and then secured with fine sutures or tissue glue. A dressing or stent may be used to protect the area during healing. Recovery can vary depending on the size and location of the graft, but patients may need voice rest, antibiotics, and regular monitoring to ensure graft success. The donor site typically heals in 1–2 weeks and may feel like a scrape or mild burn. Graft survival is usually excellent when kept moist and undisturbed.
Laryngeal stenting keeps the airway open after surgery or injury, especially in patients with laryngeal collapse, scarring, or after reconstructive procedures. A stent — typically made of silicone — is placed inside the larynx to maintain space and support healing tissues.
This procedure is done under general anesthesia and is often part of a larger reconstructive surgery. Depending on the treated condition, the stent remains in place for several days to weeks. Patients may have limited voice use or require alternative communication methods during this time. They are closely monitored for stent displacement, irritation, or infection. Once healing is sufficient, the stent is removed in a follow-up procedure. Voice and airway function are then reassessed, and additional therapies like voice training or minor revision surgery may be needed.
Foreign body removal is an emergency or urgent procedure to extract objects accidentally inhaled or swallowed. Children are most often affected, but adults can also aspirate or ingest items such as food, bones, dental appliances, or small objects. Depending on where the item is lodged — the larynx (voice box), trachea (windpipe), or esophagus (swallowing tube) — symptoms may include coughing, choking, wheezing, pain, or inability to swallow or speak.
The procedure is done under general anesthesia using a rigid or flexible scope and grasping tools. The surgeon carefully removes the object while minimizing trauma to the delicate airway and surrounding tissues. Most patients recover quickly and resume normal activities shortly after. Rare complications include bleeding, swelling, or vocal changes, especially if the object was sharp or in place for a long time. Follow-up depends on the situation but may involve imaging or repeat endoscopy to ensure no remaining injury.
This procedure opens narrowed airways (a condition called stenosis) and removes abnormal tissue that may be blocking airflow. It's commonly performed in patients with scar tissue, tumors, or inflammation in the trachea or bronchi. The goal is to restore normal breathing, reduce symptoms like wheezing or shortness of breath, and prevent airway collapse.
The procedure is done under general anesthesia. A bronchoscope — a thin, flexible, or rigid tube with a camera — is inserted through the mouth or nose into the windpipe. If there is a narrowing, a balloon or mechanical dilator is used to widen the airway. Any obstructive tissue is then carefully removed with surgical instruments or a laser. Afterward, the patient is monitored for swelling or breathing difficulty. Recovery is generally quick, though voice and breathing may differ for a few days. Some patients with chronic narrowing may need repeat procedures or follow-up imaging to maintain results.
This procedure combines diagnosis and treatment for conditions affecting the esophagus — such as trouble swallowing (dysphagia), muscle spasms, strictures, or suspected growths. Using a long, flexible scope, the doctor inspects the inside of the esophagus, collects tissue samples if needed (biopsy), injects Botox to relax tight muscles, and stretches narrowed sections (dilation) to improve swallowing.
The procedure is typically done under general anesthesia. A small camera is passed through the mouth and down the throat. Biopsies may be taken for testing. Botox is injected into areas where the esophagus is overly tight, often helping ease spasms or achalasia. Dilation is performed using inflatable balloons or soft dilators. Patients may have a sore throat afterward and must avoid eating or drinking for a few hours. Botox effects develop over a few days and can last several months. Follow-up depends on the underlying condition, but most patients experience a noticeable improvement in swallowing comfort.
 YouTube Channel
YouTube Channel