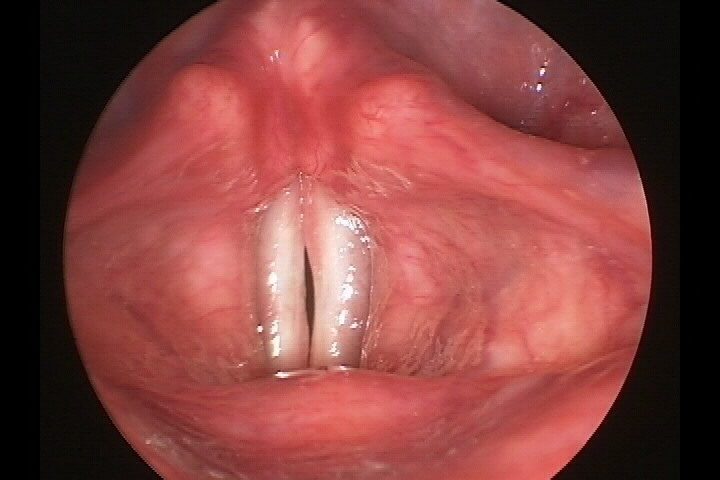
Acute laryngitis occurs when the vocal cords become swollen and irritated, leading to hoarseness, throat discomfort, and sometimes a dry or mildly productive cough. Viral infections, similar to the common cold, may cause it. Still, it can also result from voice overuse (like yelling or singing too much), allergies, acid reflux, or exposure to smoke and pollution. When the vocal cords swell, they vibrate differently, making the voice sound raspy or weak.
Most cases of acute laryngitis resolve independently within a week or two. Resting the voice, staying well-hydrated, using a humidifier, and avoiding irritants (such as smoking and alcohol) can help with recovery. Over-the-counter pain relievers and throat lozenges may also provide relief. If hoarseness lasts longer than two weeks, seeing a doctor to rule out more serious conditions is important. In some cases, bacterial infections may cause laryngitis, requiring antibiotics, though this is less common. If left untreated, repeated episodes of acute laryngitis can contribute to chronic voice problems.
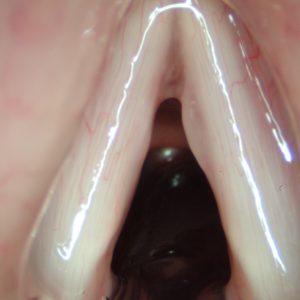
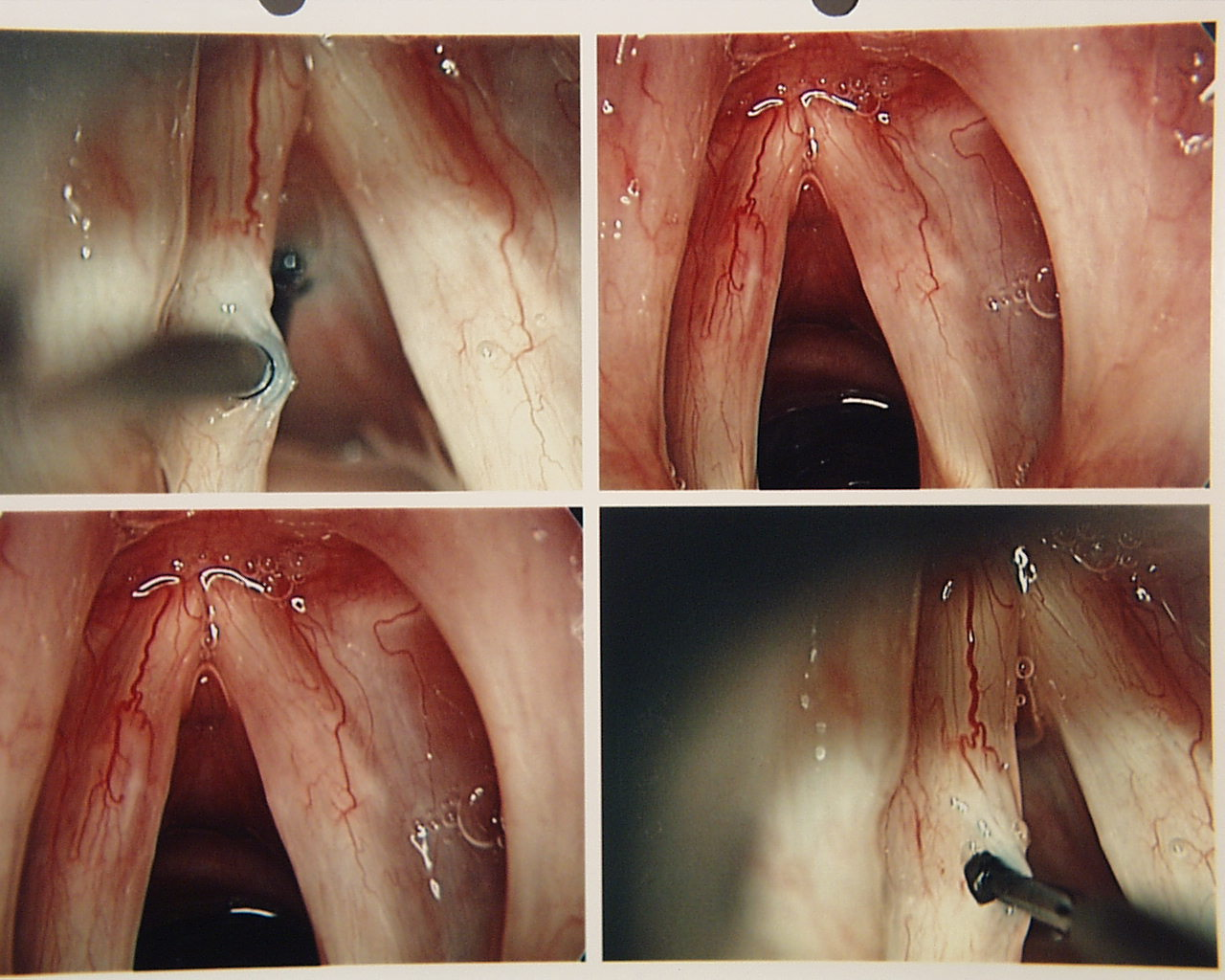
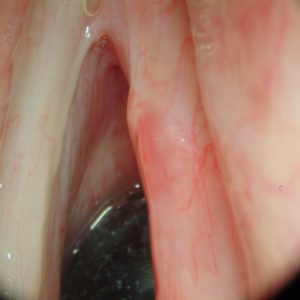
If the voice does not improve after two weeks, a laryngologist should evaluate the vocal fold function for vocal fold bleeding.
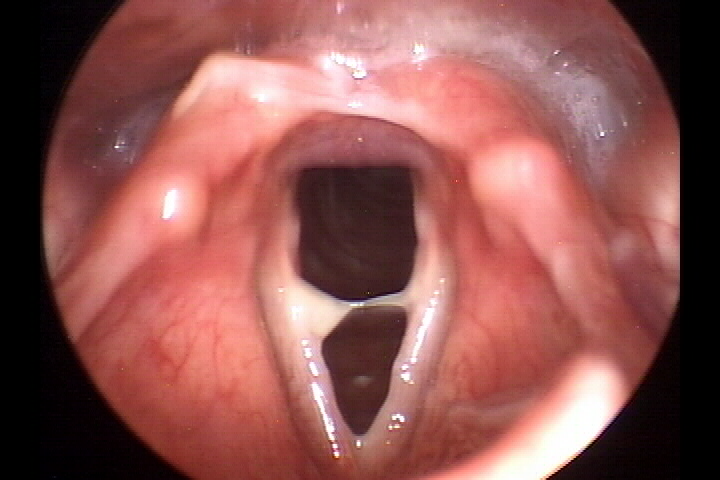
Acute Laryngitis
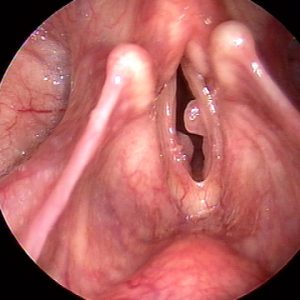
Chronic laryngitis is long-term inflammation of the vocal cords that causes ongoing hoarseness, throat discomfort, and voice fatigue. Unlike acute laryngitis, which usually resolves in a few weeks, chronic laryngitis persists for months and often results from repeated irritation. Common causes include smoking, long-term exposure to air pollution, chronic acid reflux (where stomach acid irritates the throat), frequent alcohol consumption, and vocal strain from excessive speaking or singing. Some medications, like inhaled steroids for asthma, can also contribute to chronic laryngitis.
Symptoms include persistent hoarseness, a dry or sore throat, a feeling of a lump in the throat, and increased effort needed to speak. The voice may sound deeper, rougher, or more strained than usual. If left untreated, chronic laryngitis can lead to lasting damage, including thickening of the vocal cords, scarring, and even developing vocal nodules or polyps. Treatment depends on the cause: quitting smoking, managing acid reflux, staying hydrated, avoiding irritants, and using proper vocal techniques can help. A specialist may recommend voice therapy or other medical treatmentsif symptoms persist.
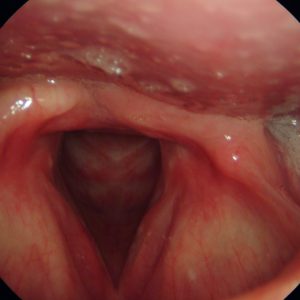
Chronic Laryngitis
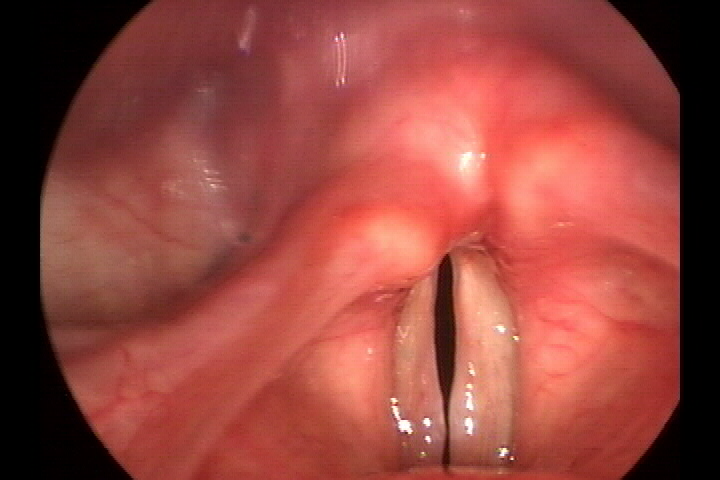
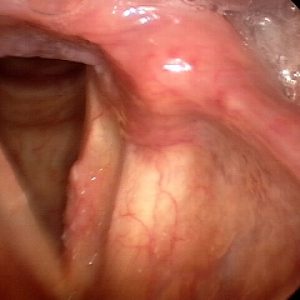
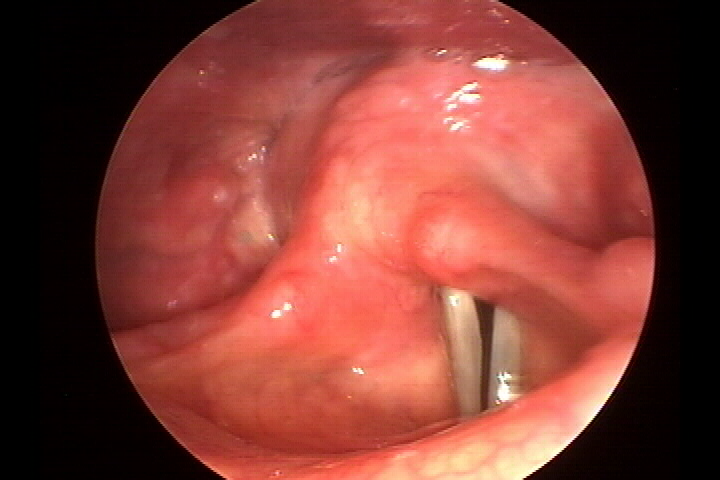
Reflux laryngitis happens when stomach acid travels into the throat and irritates the vocal cords, leading to inflammation, hoarseness, and discomfort. This condition is different from regular acid reflux (GERD) because it doesn’t always cause heartburn. Instead, patients often experience symptoms like frequent throat clearing, a persistent cough, a sensation of something stuck in the throat (Globus sensation), and voice changes.
Acute reflux laryngitis may occur occasionally, such as after overeating or drinking alcohol late at night. It usually resolves within a few days with simple changes like avoiding acidic foods, eating earlier in the evening, and sleeping with the head elevated. However, chronic reflux laryngitis happens when acid exposure becomes a long-term issue, leading to ongoing damage to the vocal cords. Over time, this can cause thickening of the vocal cords, constant throat irritation, and difficulty speaking.
Treatment involves dietary and lifestyle changes, such as avoiding spicy, acidic, or fatty foods, quitting smoking, and maintaining a healthy weight. Doctors may also prescribe acid-reducing medications like proton pump inhibitors (PPIs) for long-term control. If untreated, chronic reflux laryngitis can contribute to lasting vocal scarring and permanent voice loss.

Laryngeal Pharyngeal Reflux (LPR)

Severe Laryngeal Pharyngeal Reflux
Radiation laryngitis is a condition that affects people who have undergone radiation therapy for cancer in the head and neck area. While radiation helps destroy cancer cells, it can also cause long-term damage to healthy tissues, including the vocal cords. Radiation-related laryngitis leads to hoarseness, a weak or breathy voice, and, in severe cases, difficulty speaking. Early on, radiation can cause swelling and irritation, but over time, the vocal cords may become stiff and scarred, limiting their ability to vibrate correctly.
Symptoms of radiation laryngitis can appear weeks, months, or even years after treatment. People may notice their voice becoming progressively weaker, rougher, or more effortful. Some may experience dryness and a constant need to clear their throat due to reduced saliva production. Treatment focuses on maintaining vocal health through hydration, humidifiers, and gentle vocal exercises. Speech therapy can help patients adapt to voice changes and develop techniques to reduce strain. Treatments like steroid injections or voice implants may sometimes improve vocal function.
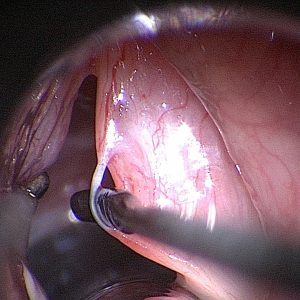
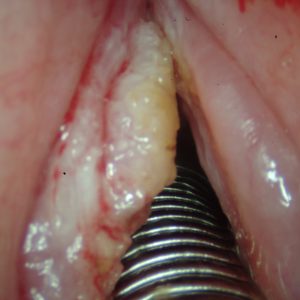
Candida laryngitis is a fungal infection of the vocal cords caused by an overgrowth of Candida, a type of yeast that naturally exists in the body. It is most commonly seen in people using inhaled steroid medications for asthma or COPD, those with weakened immune systems, or individuals who have recently taken antibiotics, which can disrupt the body's natural balance of microbes.
Symptoms of candida laryngitis include persistent hoarseness, throat discomfort, difficulty speaking, and sometimes white patches on the vocal cords or throat. Unlike bacterial infections, it does not cause fever, but the voice may feel weak and strained. Sometimes, it is mistaken for chronic laryngitis or other conditions because the symptoms overlap.
Treatment usually involves antifungal medications. If the infection is linked to inhaled steroids, patients may be advised to rinse their mouth and throat after using their inhaler to reduce the risk of fungal overgrowth. Improving overall immune health, staying hydrated, and avoiding unnecessary antibiotic use can also help prevent candida laryngitis from recurring.
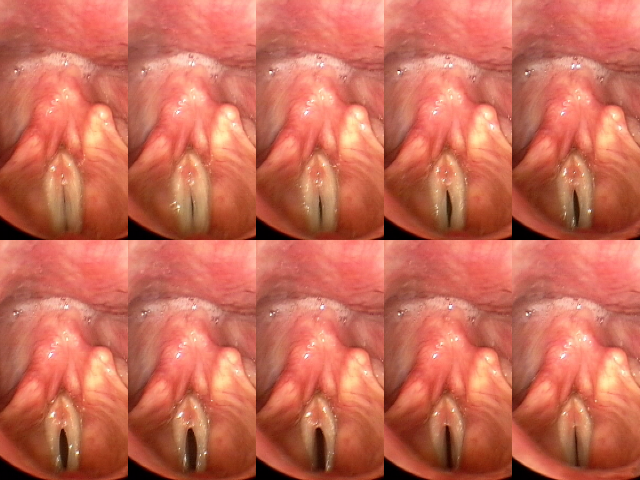
Vocal nodules are small, callous-like growths that form on both vocal cords due to repeated strain over time. They typically develop gradually in people who use their voice heavily—like teachers, singers, or public speakers. The most common causes include vocal overuse, poor technique, and untreated reflux. Patients often notice a hoarse, raspy, or breathy voice that worsens with use and improves with rest. Some may feel vocal fatigue, loss of vocal range, or tightness when speaking. Treatment focuses on behavioral changes and healing the tissue without surgery. We begin with voice therapy to reduce strain, along with hydration and reflux management. If inflammation persists, an in-office steroid injection may be used. Surgery is rarely needed unless nodules fail to respond to therapy. Recovery takes several weeks, and most patients improve fully with conservative treatment.
Vocal Fold Nodule
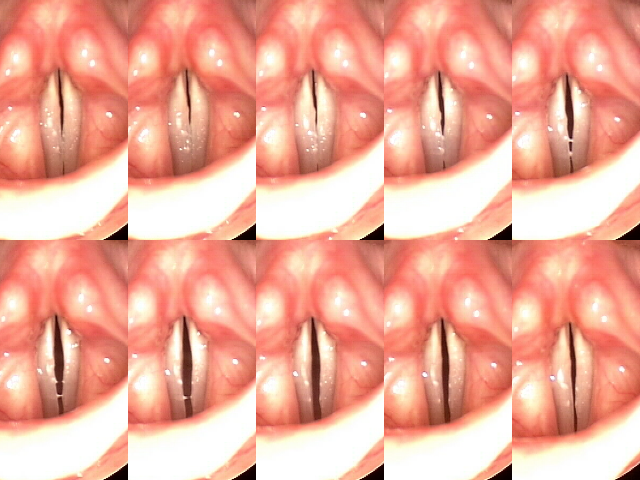
Vocal Fold Nodule in Vibration
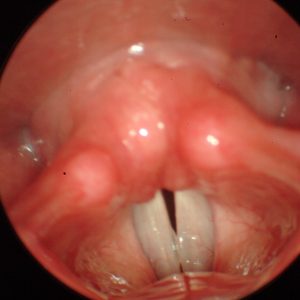
Vocal polyps are soft growths that usually develop on one vocal fold and can appear suddenly or gradually. They are commonly caused by a single traumatic vocal event (like shouting or heavy coughing), but ongoing voice strain, reflux, and smoking can also contribute. There are several types of polyps, and they differ based on how they form and how long they’ve been present.
A hemorrhagic polyp happens suddenly when a blood vessel bursts inside the vocal fold—often during a single loud yell or intense vocal effort. It fills with blood and can cause immediate hoarseness or loss of voice. A fusiform polyp is longer and sausage-shaped, forming gradually from chronic voice overuse, especially without vocal rest. A fibrotic polyp is dense and firm, usually the result of an older hemorrhagic polyp that healed poorly over time.
Symptoms of all polyps include hoarseness, a rough or uneven voice, vocal fatigue, or the feeling of something stuck in the throat. Small polyps may shrink with strict voice rest, hydration, and anti-inflammatory measures. However, persistent polyps often require microlaryngoscopy for precise surgical removal. In some cases, a blue laser or KTP laser may be used to minimize damage and speed recovery. Most patients heal in 1–2 weeks and benefit from voice therapy afterward to prevent recurrence.
Fusiform Polyp
Vocal fold cysts are small, fluid- or keratin-filled sacs that form beneath the surface of the vocal fold. Unlike nodules or polyps, cysts are located deeper in the tissue and typically do not respond to voice therapy alone. Some cysts are congenital (present from birth), while others develop from chronic vocal strain or glandular blockage.
Keratin cysts, also called epidermoid cysts, contain thick, skin-like debris and are usually present from birth or develop after vocal trauma that damages the lining of the vocal fold. These tend to be firmer and more disruptive to voice quality. Mucous retention cysts form when a mucus gland duct becomes blocked—often due to inflammation, reflux, or smoking—and they contain a thinner, watery fluid. Mucous cysts may fluctuate in size and occasionally improve with reflux treatment, but most cysts eventually require surgery.
Common symptoms include hoarseness, a weak or breathy voice, and a loss of vocal clarity or range. We treat cysts with microlaryngoscopy to carefully remove the lesion while preserving surrounding tissue. After surgery, voice rest is followed by therapy to help restore vocal function and prevent scarring. Recovery typically takes about one to two weeks, with gradual voice improvement thereafter.

Cyst
A pseudocyst is a fluid-filled swelling that appears on the vocal fold surface, often fluctuating in size depending on vocal use. It typically develops from overuse and may improve with rest. In contrast, a fibrovascular lesion is a firmer, more organized growth that develops from chronic irritation and contains fibrous and blood vessel components. These lesions may cause hoarseness, vocal fatigue, or effortful speaking. Pseudocysts may come and go, while fibrovascular lesions often persist. Treatment includes voice therapy, reflux control, and careful monitoring. If symptoms persist or interfere with speech, we may perform microlaryngoscopy for surgical removal. Both types generally heal well with appropriate care.
Pseudocyst
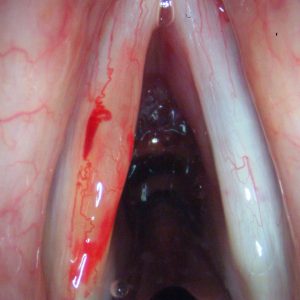
An acute vocal fold hemorrhage occurs when a blood vessel in the vocal fold ruptures, usually from vocal trauma like yelling or heavy singing. This causes blood to collect in the vocal fold, stiffening the tissue and interrupting normal vibration. Symptoms include a sudden loss of voice, hoarseness, or vocal pain. Singers may notice they can no longer hit high notes or produce sound. Immediate voice rest is essential to prevent permanent damage. We often recommend oral steroids and follow the injury closely with laryngoscopy. If blood does not resolve or if damage leads to polyp or cyst formation, surgery may be required. Recovery after surgery is typically 1–2 weeks with rest and follow-up therapy.

Vocal Fold Hemorrhage
Sulcus vocalis is a groove or indentation in the vocal fold that affects its ability to vibrate properly. It can be congenital or develop over time from chronic inflammation or prior vocal fold trauma. Because the groove is often subtle, it may go undiagnosed until the voice becomes significantly affected. Patients report a weak, breathy, or strained voice, often with limited vocal endurance. Voice quality may not improve with therapy alone. Treatment depends on severity. In mild cases, voice therapy may help improve compensation. For more significant sulci, we offer microlaryngoscopy with injection of PRP, fat, or hyaluronic acid to improve vocal cord vibration. Recovery is gradual, and therapy plays an important role before and post-procedure.
Sulcus Vocalis
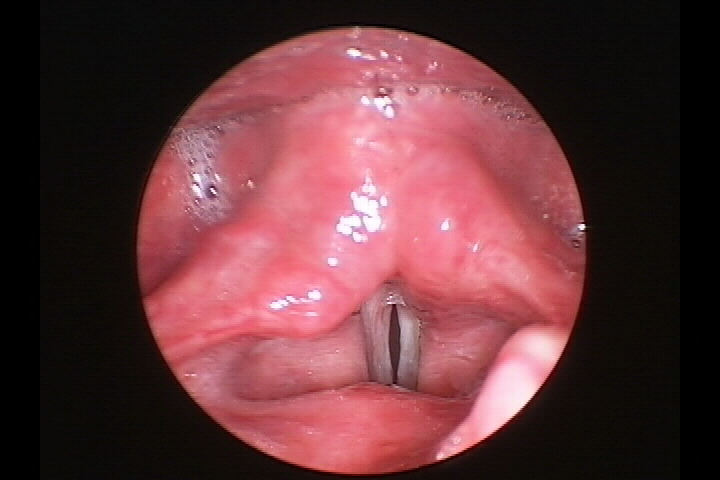
Reinke’s edema is a condition where fluid builds up in the superficial layer of the vocal fold, making it swollen and floppy. It develops slowly, often over years, and is most commonly seen in smokers and individuals with chronic acid reflux or vocal overuse. The vocal folds become thickened and lose their normal vibration, causing a deep, rough, or husky voice. In more advanced cases, the swelling can interfere with breathing. Patients typically notice that their voice sounds deeper or more strained, especially in the morning. Women may report sounding “masculine” or losing the ability to project their voice. Treatment involves quitting smoking, controlling reflux, and resting the voice. In-office steroid injections may help reduce inflammation. For more advanced cases, we may perform microlaryngoscopy to remove the excess fluid and restore the vocal folds’ shape. Voice rest is required post-surgery, and recovery usually takes 1–2 weeks.
Microwebs are thin bands of tissue that form between the vocal cords, either congenitally or following surgery or trauma. These webs may cause mild to moderate voice symptoms, depending on their size and location. Most patients report a weak, high-pitched, or breathy voice. Small microwebs may not need intervention, especially if voice quality is unaffected. For larger webs that interfere with vibration or breathing, we may recommend microlaryngoscopy to divide the tissue. Recovery typically includes a few days of voice rest and, in some cases, a temporary stent to prevent re-scarring.

Congenital Microweb
Vascular ectasia refers to enlarged or fragile blood vessels on the vocal folds, often due to long-term vocal strain, aging, or hormonal changes. These dilated vessels can rupture with vocal stress, increasing the risk of hemorrhage. Patients may notice a rough, unstable, or breathy voice and may be at risk of sudden vocal fold bleeding. Treatment focuses on reducing the risk of rupture. This includes voice therapy, reflux control, and in some cases, laser therapy. We often use blue laser or KTP laser to shrink these fragile vessels in the office or during microlaryngoscopy. Voice rest is recommended post-procedure, and most patients recover fully within a week.
A mucosal bridge is a thin band of tissue stretched over the vocal fold, usually from birth or secondary to a cyst rupture. It can interfere with normal vocal fold movement and vibration. Patients may experience a rough, strained, or unstable voice. If the bridge is small and not affecting the voice, no treatment is necessary. If it causes persistent voice changes, we may remove it during microlaryngoscopy. Recovery involves several days of voice rest followed by therapy to restore vocal function.
Mucosal Bridge
GPA is a rare autoimmune disease that causes inflammation in small blood vessels throughout the body, especially in the lungs, kidneys, sinuses, and airway. When it affects the voice box (larynx), it usually causes subglottic stenosis, or narrowing just below the vocal cords. This can lead to hoarseness, noisy breathing (stridor), shortness of breath, or frequent throat infections. Symptoms can build slowly, and it may first look like stubborn laryngitis. Because GPA is a systemic disease, it’s usually treated with oral steroids, immune-suppressing pills, and sometimes biologic drugs (prescribed by a rheumatologist). In our office, we can help manage the laryngeal symptoms with in-office steroid injections and airway dilations to open the narrowed area. In more advanced cases, a surgical airway procedure may be needed, though we try to avoid that with early intervention.
Sarcoidosis is an autoimmune disease that causes inflammatory nodules (granulomas) to form in multiple parts of the body, especially the lungs, lymph nodes, and skin. It can also affect the larynx, leading to symptoms like hoarseness, breathing difficulty, a muffled voice, and swelling in the throat. The changes can be gradual and are sometimes mistaken for allergies or reflux. In early stages, oral or inhaled steroids are often effective. When sarcoidosis causes swelling or narrowing in the larynx, we can help manage it with in-office steroid injections, and in some cases, CO2 laser treatment or dilation procedures to open the airway. We work closely with other specialists if the disease affects other organs.
Rheumatoid nodules are firm bumps that develop on the vocal cords in people with rheumatoid arthritis or other autoimmune diseases like lupus. These diseases affect the joints, but can also cause vocal fold inflammation. These nodules usually grow slowly and can cause hoarseness, vocal fatigue, or voice breaks that come and go. Treatment starts with managing the underlying disease through oral medications prescribed by a rheumatologist. In our office, we evaluate the nodule with rigid laryngoscopy and stroboscopy. If needed, we may perform an in-office steroid injection or proceed with surgical removal under general anesthesia if the nodule is large or the nodules stiffens the vocal cord.

Rheumatoid Nodule

Rheumatoid Nodule
Pemphigus is a rare autoimmune blistering disease that typically starts in the skin or mouth but can also affect the throat and voice box. When it involves the larynx, it can cause painful sores, hoarseness, coughing, throat bleeding, and even scar tissue that narrows the airway. Related diseases include pemphigoid and cicatricial pemphigoid, which can also cause mucosal scarring in the throat. Pemphigus is usually managed with oral or intravenous steroids, and immune-suppressing medications coordinated with a dermatologist or rheumatologist. In our office, we help manage airway symptoms with CO2 laser treatment, injections, or dilation to open any scarred areas. If airway narrowing becomes severe, we may recommend surgery or, in rare cases, a tracheostomy.
While Crohn’s disease and ulcerative colitis primarily affect the digestive tract, they can occasionally cause inflammation in the throat or larynx. Patients may notice sore throat, hoarseness, or a burning sensation in the throat during a digestive flare-up. These cases are uncommon and usually resolve once the bowel disease is under control. We can evaluate the larynx to rule out other causes of inflammation. If needed, we may prescribe a short course of oral or inhaled steroids, but usually, no procedures or surgeries are required.
Aphthous ulcers are small, shallow sores that can develop in the mouth or throat, including the larynx. They are not part of a systemic disease and usually appear during times of stress, illness, or immune suppression. They can cause mild pain, irritation, and frequent throat clearing, but they don’t block the airway. Treatment is simple and supportive. In our office, we may recommend saltwater gargles, topical treatments, or expectorants to soothe the area. These ulcers usually go away on their own within 1–2 weeks, and no surgery or procedure is needed.
Contact granuloma is a growth of inflammatory tissue that forms on the vocal process of the arytenoid cartilage—where the vocal folds come together—typically due to repeated irritation. This irritation can come from forceful voice use, chronic throat clearing, or acid reflux. Patients often feel a tickle or lump in the throat, persistent hoarseness, and pain when speaking, usually on one side. Over time, the lesion can grow and become large enough to affect vocal quality or breathing. It often develops gradually in people who speak loudly, forcefully, or for long periods, especially men.
Treatment usually begins in the office. Voice therapy is recommended to reduce strain, and patients are started on aggressive acid reflux control. Inhaled or injected steroids may be used to reduce inflammation. In some cases, Botox injections into the vocal muscles are offered to temporarily relax the area and allow healing. If the granuloma is large, painful, or obstructing the airway, it may be removed surgically under general anesthesia. The granuloma can also be precisely treated with a blue laser or KTP laser, either in-office or in the operating room. Recovery involves voice rest, reflux management, and regular monitoring to prevent recurrence.

Contact Granuloma

Contact Granuloma
Intubation granuloma is a type of vocal lesion that forms after a patient has been intubated—when a breathing tube is inserted during surgery or hospitalization. The pressure or movement of the tube can irritate the tissue at the back of the voice box, especially if the tube was in place for a long time. These granulomas usually appear a few days or weeks after the hospital stay. Patients may notice new hoarseness, breathiness, or even a weak or absent voice.
These lesions can be quite large, but often respond well to conservative treatment. In our office, we typically begin with high-dose acid reflux medications, inhaled or oral steroids, and careful monitoring. If the granuloma does not improve or if it affects breathing, we may recommend blue laser or KTP laser ablation, which can often be done in the office. In rare cases, if the lesion causes airway obstruction, surgical removal under general anesthesia may be necessary. Most patients recover fully with non-surgical care and ongoing voice and reflux management.
A contact ulcer is a painful sore that develops on the vocal process—the point where the vocal cords meet—usually from chronic irritation. It is often an early stage in the same process that leads to a contact granuloma. The ulcer may be caused by voice overuse, excessive throat clearing, or acid reflux, and typically occurs on one side of the throat. Patients with a contact ulcer often report a sharp pain during speaking or swallowing, and may feel like something is stuck in their throat. Hoarseness and a dry, irritated throat are also common. These ulcers develop slowly and can become more painful over time if not addressed. Treatment does not usually involve surgery. Instead, we focus on stopping the irritation: this includes voice therapy to change speaking patterns, non-acid and acid reflux treatment, and sometimes an inhaled or injected steroid to reduce inflammation. If treated early, contact ulcers usually heal without the need for further intervention.
Osteosclerosis of the arytenoid cartilage is a hardening or thickening of the cartilage at the back of the voice box. This condition may not be visible on a basic exam, but can be seen on a CT scan. It is most often discovered in patients who have recurrent contact granulomas that don’t improve with treatment. The hardened cartilage can press against the opposite vocal cord and prevent the area from healing properly. Patients with osteosclerosis may feel hoarseness, vocal fatigue, or discomfort on one side of the throat. Because it causes mechanical irritation, even a small area of thickening can lead to repeat trauma with every vocal fold closure. Treatment begins with reflux control and may include steroid injections or antibiotics if there is inflammation. In rare, persistent cases, surgery may be needed to reshape or reduce the thickened cartilage. Recovery depends on the severity of the disease and may include continued voice therapy and close follow-up.
An arytenoid dislocation happens when one of the small cartilages in your voice box, called the arytenoid cartilage, gets moved out of its usual place. Arytenoid dislocation can occur because of a rough intubation (when a breathing tube is placed) or a hard hit to the throat. When the arytenoid is out of place, you might notice a hoarse, breathy voice, throat pain, or trouble swallowing. Sometimes, its symptoms can seem very similar to vocal cord paralysis, even though the issue is actually the misplaced cartilage.
Doctors usually check for arytenoid dislocation by looking into your throat with a small camera or doing a CT scan. If they find that the arytenoid is not in its proper position, they often try to fix it with a closed reduction procedure, which gently moves the cartilage back into place. Voice rest, special injections (like Botox), or other therapies might be used afterward to help your voice improve and prevent the problem from coming back.
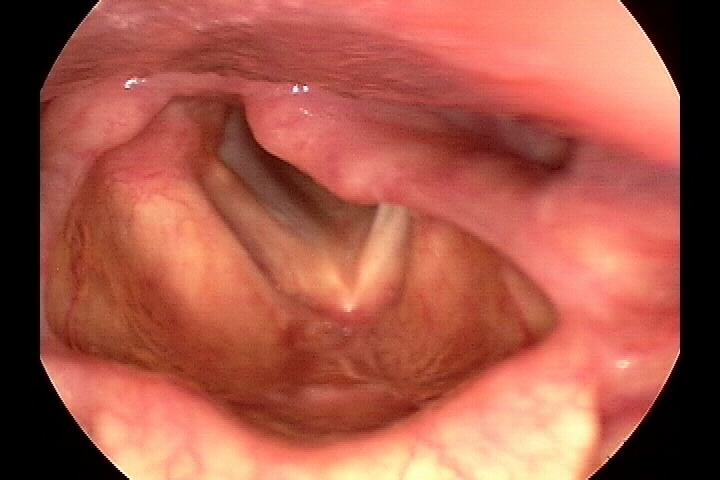
Laryngeal stenosis means that the airway in your voice box has become too narrow. This narrowing usually happens because of scar tissue that forms after long-term use of a breathing tube or after a throat injury or surgery. When the airway is narrowed, you might have trouble breathing, especially during exercise, or notice your voice becoming weak or breathy. In some cases, the narrowing can be small enough that you only feel slight changes, but in others, it can make it hard to get enough air.
Doctors use tools like endoscopy or CT scans to see exactly where and how much your airway has narrowed. Depending on the severity of the stenosis, treatment can range from medical therapy and laser procedures to more involved surgeries. The goal is to remove or reduce the scar tissue so that the airway opens up again, helping you breathe easier and restoring a better voice quality.
Laryngeal Stenosis
Vocal fold scar happens when the soft tissues in your voice box heal with extra stiff, fibrous tissue after an injury or surgery. This scar can make your vocal folds less flexible and change the way they vibrate, which may result in a hoarse, weak, or breathy voice. The scar forms when the usual layers of the vocal fold are disrupted and heal abnormally, and even though the scar may look fine under regular light, special tests (like stroboscopy) can show that the vibration is not as smooth or strong as it should be.
Understanding the healing process of the vocal folds is crucial. In the early stage, inflammation and new tissue growth occur as the body tries to repair the injury. The key is early intervention. If the vocal folds heal quickly (called primary healing), the surface layer can grow back smoothly, preserving some of the natural flexibility. However, if the healing is slower or involves more tissue damage (secondary healing), extra scar tissue can form, leading to stiffness and less voice quality. The extent of the surgery and the specific layer affected play a significant role in how much scar forms and how it impacts your voice.
Rehabilitation strategies for vocal fold scars are a collaborative effort between doctors and speech therapists. These professionals work together to devise a plan that may include voice therapy, gentle vocal exercises, and sometimes steroid injections to reduce inflammation and prevent thick scar formation. The ultimate goal is to maintain the softness and flexibility of the vocal folds during the healing process. Newer therapies, such as regenerative medicine, are also being explored, including the use of platelet-rich plasma (PRP) and stem cell therapy.
With proper care and the right rehabilitation strategies, many patients experience significant improvements in their voice quality, although it might not return to exactly how it was before the injury or surgery. This potential for improvement offers hope and optimism to those dealing with vocal fold scars.
Vocal Fold Scar
Vocal Fold Scar
Leukoplakia is a condition where thick white or red patches form on the surface of the vocal cords. These patches are caused by irritation or damage to the top layer of the vocal cords. Common causes include smoking, acid reflux, and long-term voice overuse. These lesions may be reactive due to irritation, but sometimes they can be precancerous, which means they have the potential to turn into cancer if left untreated. Rarely is it cancerous.
Many people with leukoplakia notice that their voice sounds hoarse, rough, or weak. You might feel like you're straining to speak, or that your voice tires out more easily. Some people lose their vocal range, especially when trying to sing or speak loudly.
Your doctor will first look at your vocal cords using a small camera, often with a technique called stroboscopy to check how your vocal cords move. If the white patch looks concerning, your doctor may recommend a biopsy—this means taking a small piece of the lesion to look at under a microscope.
If the lesion is on the surface and not too deep, it can sometimes be treated right in the office using a laser (like a blue laser or KTP laser). The doctor uses a thin scope through the nose and a precise laser to remove the patch. This is done with numbing medicine, and you're awake but comfortable during the procedure. If the lesion is larger or deeper, it may need to be removed in a surgical procedure at a hospital or surgery center. This is called an outpatient procedure, which means you go home the same day—no overnight stay is needed.
Most people recover within a few days to a week. Your doctor may recommend voice rest (no talking or whispering for a short time) to help your vocal cords heal. You'll also be advised to stop smoking or treat acid reflux if those are contributing factors. Regular check-ups are important because leukoplakia can come back.
Benign keratosis is a condition where the surface of the vocal cords becomes thick and rough. It often looks like white patches, and the texture may appear bumpy or wart-like. This happens when the top layer of the vocal cords responds to long-term irritation—commonly from smoking, acid reflux, voice overuse, or environmental exposure like air pollution or chemicals. “Benign” means it’s not cancer, but the condition still needs to be monitored because it can sometimes change or worsen.
Benign keratosis usually develops slowly over many months or years, so the voice changes may sneak up on you. People often notice increasing hoarseness, raspiness, or vocal fatigue. You might feel like your voice is rough, strained, or weak, and your vocal range may become more limited—especially if you sing or speak a lot. While the condition itself forms gradually, some people experience a more sudden change in voice if the lesion thickens significantly, becomes irritated, or is associated with a cold or heavy voice use.
Your doctor will examine your vocal cords using a small camera and may use stroboscopy to check how well your vocal cords vibrate. If the lesion looks clearly benign and isn’t affecting your voice too much, your doctor may suggest watchful waiting, along with lifestyle changes like quitting smoking or treating acid reflux.
For surface-level keratosis, the doctor may use a laser (like a blue laser or KTP laser) during an in-office procedure. You’ll be awake but your throat will be numbed, and a small flexible scope is used through your nose to treat the lesion precisely. If the lesion is thicker, or if a full biopsy is needed to examine it more closely, your doctor may recommend an outpatient surgery—a short procedure under general anesthesia where you go home the same day.
Most people recover within a few days to a week. Voice rest is usually recommended, and your doctor may talk to you about avoiding irritants like smoking, acid, or heavy voice use. Regular follow-up is important. The keratosis can return or change over time.

Keratosis
Laryngeal cancer is a type of throat cancer that affects the voice box (larynx). It can develop when abnormal cells in the vocal cords grow uncontrollably, forming tumors. The exact cause is not always known, but smoking, heavy alcohol use, and exposure to certain chemicals can increase the risk. Symptoms often include a persistent hoarse voice, difficulty swallowing, and a lump in the throat. Doctors use specialized tools, like video stroboscopy (a procedure that uses a strobe light to examine the vocal cords), to examine the vocal cords and determine whether the cancer is affecting only the surface or has spread deeper into the tissue.
When laryngeal cancer is found early, it can be treated by An ear, nose, and throat (ENT) surgeon. These specialists are trained to diagnose and treat conditions of the head and neck, including the larynx. They can treat this with minimally invasive procedures. One standard method is transoral laser surgery, where a surgeon carefully removes the affected tissue using a laser. If the cancer is more advanced, deeper layers of the vocal cords may need to be removed, which can impact the voice. Radiation therapy is another treatment often used for early cancer. Stroboscopy helps doctors decide how much tissue to remove while preserving as much voice function as possible. In some cases, more extensive surgeries like a partial or total laryngectomy (removal of part or all of the voice box) may be needed.
Recovery from laryngeal cancer is a journey that depends on the type and extent of treatment. While patients may experience temporary hoarseness for minor procedures, they can return to normal activities fairly quickly. For those who undergo more significant treatments, such as the removal of a portion of the vocal cords, voice therapy becomes a crucial part of the recovery process. This therapy not only aids in speech but also instills hope and optimism for a restored voice. Avoiding smoking and alcohol, following a healthy diet, and attending regular check-ups are essential for preventing recurrence. Remember, early detection and treatment give the best chances of preserving the voice and overall health.
Cancer

Verrucous Cancer
Pre-cancer
Vocal atrophy is a condition that affects the voice as people age. It happens when the muscles inside the voice box (larynx) weaken and lose mass, making the vocal cords thinner and less able to close correctly. Vocal atrophy can cause a weak, breathy voice that lacks power and clarity. Vocal atrophy differs from general aging-related voice changes, known as presbyphonia, because it refers explicitly to the thinning and weakening of the vocal folds. Factors like aging, illness, weight loss, and reduced use of the voice can contribute to this condition.
The effects of vocal atrophy on daily life can be significant. People with this condition often find that their voice becomes softer and more challenging to hear, especially in noisy places. They may feel like their voice is unreliable, becoming weaker or fading as the day progresses. Some may develop a slightly raspy or muffled voice quality and experience vocal fatigue. Doctors diagnose vocal atrophy by examining the vocal cords with unique cameras that show how they vibrate. These exams often reveal that the vocal cords are not closing correctly, leaving gaps that cause the voice to sound weak.
Treatment for vocal atrophy usually starts with voice therapy, a highly effective method to strengthen the vocal muscles and improve breath control. If therapy alone is insufficient, doctors may recommend in-office procedures like vocal cord injections, where a substance is added to the vocal folds to make them thicker and help them close better. Regenerative therapies such as platelet-rich plasma (PRP) have been used as a minimally invasive way to treat vocal atrophy. Surgery may be needed to reposition the vocal cords in more severe cases. Recovery varies depending on the treatment, but many patients see improvements in voice strength and clarity within weeks to months. Regular vocal exercises and staying hydrated can also help maintain vocal health.
Vocal Atrophy
Vocal Atrophy
Laryngeal papillomas are small, wart-like growths that develop in the voice box (larynx) due to the human papillomavirus (HPV). These growths can cause hoarseness, difficulty breathing, and a rough or strained voice. While papillomas are not cancerous, they can grow back even after treatment, sometimes requiring repeated procedures. Children and adults can both develop laryngeal papillomas, with young children often having more severe cases.
Treatment usually involves in-office or surgical removal of the growths using lasers or other specialized tools. Sometimes, doctors may use medications to help slow down their return. Patients might need multiple treatments to keep their airway clear and improve their voice. Recovery depends on the extent of the procedure, but most patients experience a noticeable improvement in their voice shortly after treatment. Regular follow-ups are essential to monitor for regrowth.

Papilloma
Papilloma
Verrucous lesions are rough, wart-like growths on the vocal cords that can make the voice sound hoarse, weak, or breathy. These lesions are often caused by long-term irritation, such as smoking, acid reflux, or chronic vocal strain. Some verrucous lesions are harmless, but others may be linked to early-stage cancer, making proper diagnosis important.
Doctors typically examine the vocal cords using a camera-based procedure called laryngoscopy to determine the nature of the lesion. If needed, a biopsy is performed to rule out cancer. Treatment depends on the cause, but options may include laser removal, voice therapy, and lifestyle changes like quitting smoking or managing acid reflux. Recovery varies, but patients usually experience voice improvement within weeks after treatment.
Laryngoceles are air-filled sacs that develop in the larynx. They can be internal, staying within the voice box, or external, extending outward. These sacs form when mucus glands become blocked or due to increased pressure from activities like playing wind instruments or frequent coughing. If external, laryngoceles can cause hoarseness, breathing difficulties, or a visible lump on the neck.
Treatment depends on the severity of symptoms. Small, non-bothersome laryngoceles may not need treatment, but larger ones that affect breathing or cause discomfort might require surgical drainage or removal. Most patients recover well with minimal complications, and follow-up care ensures that the problem does not return.

Laryngocele
Saccular cysts are fluid-filled sacs that develop in a small pocket of the voice box called the saccule. If they grow too large, they can block normal vocal cord movement, leading to hoarseness, throat discomfort, or even breathing problems. They may form due to mucus buildup or previous infections.
Doctors diagnose saccular cysts using imaging tests or direct examination with a scope. Depending on the cyst's size and location, treatment usually involves surgical removal in an office setting or the operating room. Recovery is generally smooth, with most patients noticing improvements in their voice and breathing soon after the procedure. Voice therapy may be recommended if the cyst affects vocal cord function.

Saccular Cyst
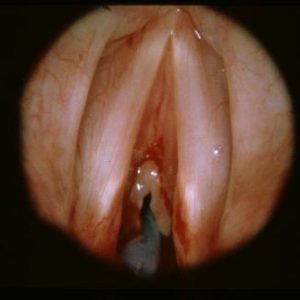
Vocal fold paralysis happens when one or both vocal cords lose their ability to move, due to damage to the nerves that control them. This can occur suddenly or gradually and may result from viral infections, surgical complications (such as thyroid or spine surgery), trauma, tumors, or neurological conditions. Sometimes, a growth in the chest, neck, or skull base can press on the nerve, especially the recurrent laryngeal nerve, causing paralysis. If this is suspected, we may order a CT scan of the neck.
When just one vocal fold is paralyzed (unilateral), the voice often sounds hoarse, breathy, or weak, and patients may feel tightness, burning, or fatigue in the throat from the muscles working too hard to compensate. Bilateral paralysis, where both vocal folds are affected, is more rare and can lead to breathing difficulties, noisy breathing (stridor), or even airway blockage in severe cases.
In our office, we use flexible laryngoscopy to view the vocal folds and sometimes additional imaging or EMG to assess nerve function. Some cases recover on their own within months, but others require treatment to improve voice and breathing. We offer in-office vocal fold injection with Restylane to help bring the paralyzed fold closer to the midline, improving voice quality and reducing strain. For long-term issues, surgical options like medialization thyroplasty, fat injection, or reinnervation may be recommended.
Vocal Fold Paralysis
Vocal Fold Paralysis
Vocal fold paresis means one or both vocal cords are weakened but not completely paralyzed. The folds still move, but not with full strength or coordination. This may be caused by viral infections, minor surgical injuries, inflammation, or may occur without a clear cause. When only one side is affected (unilateral), patients may notice a breathy, weak, or unstable voice, vocal fatigue, and sometimes a sensation of tightness or burning in the throat. When both sides are affected (bilateral), which is rare, patients may have a weak or effortful voice and difficulty breathing when active.
Diagnosis involves a laryngoscopic exam and sometimes electromyography (EMG) to assess nerve function. Many cases improve with time and voice therapy alone. In more persistent cases, we offer in-office Restylane vocal fold injections to help the folds close more efficiently. For more significant or long-standing paresis, surgery can help reposition the fold for better vocal closure. Fat injection into the vocal folds can also help with the voice. Recovery depends on the severity of the condition and typically involves follow-up voice therapy to reduce strain and rebuild healthy vocal patterns.
To read more, visit our page What is Paresis.
Irritable Larynx Syndrome (ILS), also known as neurogenic cough or chronic laryngeal cough, happens when the voice box (larynx) becomes overly sensitive, reacting too strongly to things like strong smells, smoke, allergies, or even talking too much. People with ILS often experience a persistent cough that doesn’t go away with typical treatments. They may feel like their throat is tight, dry, or irritated, and they may cough frequently or have trouble speaking. Sometimes, even normal things like laughing, breathing cold air, or eating spicy food can trigger discomfort.
Doctors believe that ILS can develop after an illness, acid reflux, or repeated exposure to irritants like smoke, perfumes, or chemicals. Chronic cough is often one of the main symptoms, and in these cases, it is considered a neurogenic cough—caused by abnormal sensitivity in the nerves that control the throat and airway. Diagnosis usually involves a doctor listening to your symptoms and sometimes using a small camera to check your throat. There’s no single test for ILS or neurogenic cough, but ruling out other conditions helps confirm it.
Treatment focuses on calming the throat and retraining the larynx to be less sensitive. This can include speech therapy, breathing exercises, avoiding known triggers, and sometimes medication to reduce irritation. In more severe cases, Botox injections or a nerve block can temporarily relax the overactive muscles in the larynx, helping to relieve symptoms like throat tightness, voice strain, and chronic cough. Managing stress and staying hydrated can also help. With the right approach, most people see significant improvement and can function comfortably.
Spasmodic dysphonia is a voice disorder caused by involuntary muscle spasms in the voice box (larynx). These spasms make the vocal cords contract too much or in an uncoordinated way. When this happens, your voice might sound strained, choppy, or even “pressed” as if you’re struggling to speak. Some people with this condition may notice that their voice sounds different when they speak normally versus when they sing or hum.
Doctors diagnose this condition by listening carefully to your speech and examining your vocal cords with a tiny camera (fiberoptic laryngoscopy). They might ask you to do tasks like sustain a vowel sound or count in a specific way. These tests help them tell the difference between the common type (adductor spasmodic dysphonia) and a less common type (abductor spasmodic dysphonia), as each affects the voice in slightly different ways.
Treatment is usually done in the doctor's office by injecting a small amount of Botox into the overactive muscles. For people with adductor spasmodic dysphonia, Botox is placed into muscles that make the vocal cords come together too tightly. For those with abductor spasmodic dysphonia, the injection goes into a muscle that usually helps open the vocal cords. These injections help relax the muscles, making your speech smoother for several months. In cases where Botox isn't enough or if a patient prefers a different approach, surgery might be considered as an alternative treatment.
A vocal tremor occurs when one's voice shakes or quivers while speaking or holding a note. This trembling happens because the vocal cords vibrate irregularly, causing the voice to sound unstable. The tremor might change in speed or strength and can sometimes be seen along with other voice issues. It is important to note that vocal tremors can appear on their own or in association with different conditions, such as essential tremors or Parkinson's disease.
Doctors use special video techniques like stroboscopy or high-speed imaging to look at how your vocal cords move when you speak. These tools help capture the rapid changes and irregularities that cause the trembling. Treatment options depend on the underlying cause but may include voice therapy, medications, or Botox injections. These approaches aim to reduce the shaking so that you can speak more steadily, and the treatment choice is based on how severe the tremor is and what might be causing it.
Some neurological conditions, such as Parkinson's disease, ALS (amyotrophic lateral sclerosis), and myasthenia gravis, can affect the nerves that control the muscles in your voice box. When these nerves don't work properly, it can lead to a weak, soft, or hoarse voice and problems swallowing or speaking clearly. These voice changes might sometimes be the first sign of a more significant neurological issue, even before other symptoms appear.
In the doctor's office, specialists use tools like video laryngoscopy and sometimes electromyography (a test that measures muscle electrical activity) to examine how well your vocal cords are moving. Treatment typically involves working closely with a team including neurologists, ear–nose–throat doctors, and speech therapists. They often recommend voice therapy to help strengthen your vocal muscles and improve your speaking clarity. In some instances, if voice therapy alone isn't enough, doctors might suggest injections or surgery to support better vocal cord function. The improvement you see depends on the overall progress of the neurological condition, but early and targeted treatment can help you maintain better communication and quality of life.
Functional dysphonia is a voice problem that is not caused by a physical injury or disease of the vocal cords. Instead, it happens when the voice is affected by stress, habits, or even psychological influences. In simple terms, the voice does not work normally because of how the muscles are used (or not) rather than because of an organic disease like inflammation or growth. Sometimes, these issues are mistakenly thought to be caused by conditions like reflux laryngitis, which can lead to the wrong treatment.
Doctors usually evaluate functional dysphonia by carefully examining how the voice sounds and examining the vocal cords with a small camera (fiberoptic laryngoscopy). They might ask you to perform different speaking tasks so they can see if your vocal cords are vibrating normally. Treatment for functional dysphonia typically involves voice therapy with a speech-language pathologist to help retrain proper voice use. In some cases, if stress or emotional factors contribute to the problem, psychological support may also help get to the root of the issue.
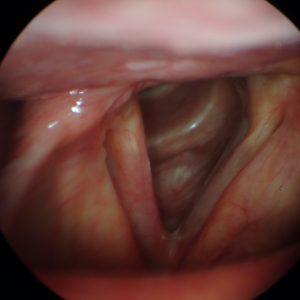
Muscle tension dysphonia (MTD) is a voice disorder that happens when the muscles around the voice box are too tight or used in a way that makes speaking difficult. This extra tension can cause your voice to sound strained, rough, or hoarse. MTD can be a primary problem or how the body compensates when there is another issue, such as swelling from reflux or scarring from a previous injury. The condition might be noticed as an abnormally high or tight-sounding voice and sometimes even physical discomfort in the neck and throat.
During an examination, doctors look for signs of tension by watching how the vocal cords move during speech and feeling tenderness in the neck muscles. Special techniques like fiberoptic laryngoscopy are used to observe patterns such as a squeezed or compressed vocal fold position. Treatment for MTD usually centers on voice therapy techniques that help you relax your laryngeal muscles and improve your breathing and speaking habits. Methods such as laryngeal massage, resonant voice therapy, and exercises to reduce unnecessary muscle tension are often used. Addressing any underlying medical issues in patients with muscle tension dysphonia is essential so that voice therapy can be the most effective.